These are not hypothetical – they’re lessons based on real patient cases, revealing the everyday habits, things dermatologists never do because they quietly damage your skin. Let’s dive in.
1. I Would Never Smoke
Why?
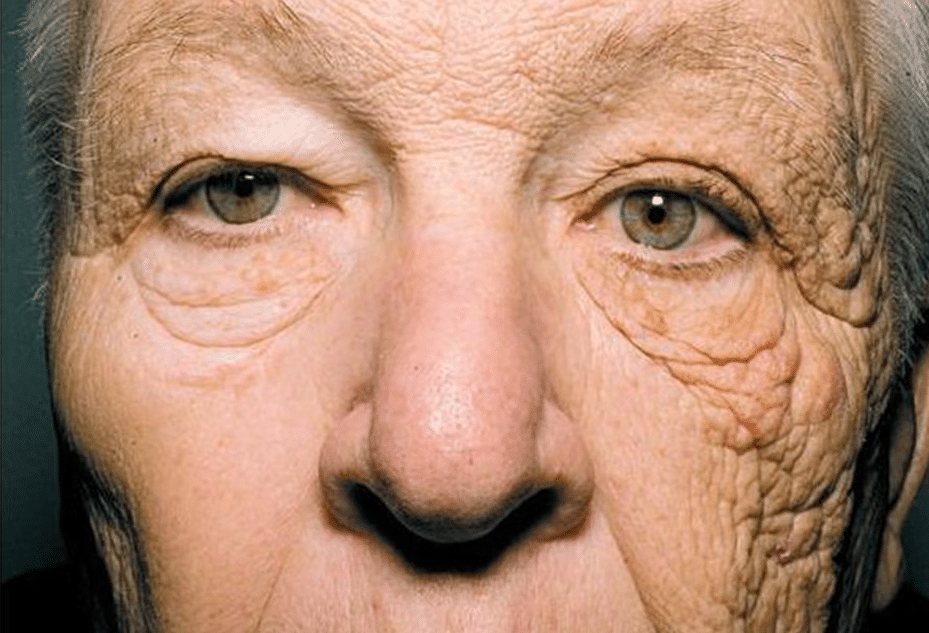
Smoking isn’t just damaging—it’s a skin ageing powerhouse:
- A Finnish study measured 18–22% lower collagen production (types I and III) in current smokers compared with never-smokers.
- Tobacco boosts collagen‑degrading enzymes (MMP-8), thinning the structural support of skin.
- Chronic exposure triggers premature facial ageing, often appearing equivalent to 20 years older in smoking decades.
- Skin tightness returns only gradually – full collagen recovery takes months after quitting.
Beyond appearance: smokers heal poorly after procedures; many surgeons decline to operate on them. Smoking also amplifies blood vessel damage, erectile dysfunction, cataracts, and cancer risks.
Clinician tip: Encourage quitting. Quitting starts collagen rebound in 4–12 weeks.
2. I Would Never Use a Tanning Bed
The problem: Tanning beds often emit 10–15× more UVA than the midday sun. UVA penetrates deep, breaking collagen and elastin and triggering free radicals.
Health impact:
- Indoor tanning raises melanoma risk by ~27% overall, up to 47% if first use is before age 20.
- Basal and squamous cell carcinoma risks also climb significantly.
- At-home ‘collariums’ marketed as safe sources of “UVA-only” light are still carcinogenic and degrade skin.
Cosmetic regret: Over the years, I’ve had countless conversations with patients who deeply regret their tanning bed use. The reason? The skin becomes severely sun-damaged, wrinkly, blotchy, and often develops a leathery texture. Many describe it as “ugly” or “aged before its time.” Sadly, by the time they seek help, the damage is often permanent, with no way to fully reverse it.
Derm take: There’s no such thing as a safe tan. Sunscreen or sunless tanner – okay. Tanning beds – no.
3. I Would Never Walk Barefoot in Public Spas or Locker-Room Showers
Why? Dermatologists treat a raft of foot infections – warts, fungal infections, verrucae – often acquired from public communal spaces.
Environment: warm, moist, and unregulated. Tap into these hotspots? You risk:
- Plantar warts (HPV virus)
- Athlete’s foot (tinea)
- Toenail fungus
- Other bacterial or viral conditions
Real-world consequence: I, as a dermatologist, treat viral warts and fungal infections almost every day in my practice. Many patients acquire these from public spas, saunas, and showers by not wearing flip-flops. And as a member of a club, I see how many people walk barefoot without realising the risk they’re taking.
My rule: Always wear protective flip-flops.

4. I Would Never Touch My Face on Public Transport
The danger: Studies show public transport surfaces can be dirtier than toilets. Despite this, people still:
- Eat on buses
- Touch handrails then rub eyes
- Skip hand washing after restroom use
Real-world consequence: I remove countless viral infections from patients’ faces every year, often caused by touching the face after unknowingly picking up a virus from contaminated surfaces. Be aware – this is a common and preventable route of transmission.
Derm take: Even if you’re healthy, frequent face-touching boosts risk of acne, viral infections, and dermatitis. Carry hand sanitiser and consciously avoid touching your face.
5. I Would Never Let My Skin Get Too Dry
The issue: Dry skin isn’t just itchy—it’s a weakened barrier.
- Animal models show moisturisers like glycerin or urea reduce trans-epidermal water loss and improve barrier function.
- A 6-week clinical trial using colloidal oatmeal moisturiser improved hydration and roughness in dry skin.
- Regular moisturising helps the skin protect itself from allergens, irritants, and infection.
Real-world consequence: Examining patients in my clinic, I often see very dry skin, especially on the legs. It makes existing conditions worse and makes skin more vulnerable to inflammation and infection. Even GPs often forget to recommend emollients. Don’t wait—moisturise. If you have any skin issues, your first action should be using an emollient. Help your skin help itself.
Derm tip: Suggest patients use at least a daily emollient with barrier-strengthening ingredients (ceramides, glycerin, colloidal oatmeal).
6. I Would Never Ignore a New or Changing Skin Lesion
Why? Melanoma and other skin cancers are dangerous—and early detection saves lives:
- Lesions that change in shape, colour, or size or start bleeding should be examined promptly.
- Even benign-looking lesions can surprise you. I’ve seen deadly melanomas dismissed as harmless.
Real-world consequence: I have sadly seen hundreds of patients die from melanoma. One of them was my childhood friend, Tamás. Most people know someone who has suffered or died from skin cancer. These tragedies are preventable—if you act early.
Derm practice: “Look before it’s too late.” Recommend annual skin checks and vigilance for any changes.

7. I Would Never Believe DIY Skincare Hacks from Social Media – Without Fact-Checking
Clarification: Social media isn’t evil – many dermatologists (myself included) share good tips online. But not everything on TikTok or Insta is safe or backed by evidence.
Case in point: I made a video debunking a trending recommendation to daily-use ‘Clinisept’ (stabilised hypochlorous solution). While HOCl does have benefits in wound care and mild dermatitis, that doesn’t mean it’s suitable for daily facial use.
Real-world consequence: Even my 18-year-old daughter often comes to me with skincare tips she finds on social media and double-checks them with me. But not everyone has a dermatologist in the family. You need to rely on your own fact-checking—and that habit could protect your health.
Mindset takeaway: Question every hack, find the proof, check studies – or ask a professional. That’s great self-care in a world of viral beauty trends. And honestly, learning to fact-check content isn’t just good for skincare – it’s good for life.
Ready to Take Your Skin Seriously?
If you’ve read this far, you’re already thinking more like a dermatologist. But if you recognise any of the following in yourself or a loved one, it might be time to take the next step:
- A stubborn growth on your sole or fingers?
- A bump or spot on your face that you keep touching?
- Ongoing dry, flaky, irritated skin that just won’t settle?
- A changing mole or new lesion that worries you?
At the Chiswick Clinic, we offer expert dermatology consultations to assess, diagnose, and treat exactly these concerns. Whether it’s a viral lesion, dry skin condition, or a suspicious mole, getting professional input early can save you pain, time, money – and in some cases, your life.
Book your dermatology consultation today and let’s make sure your skin is in safe hands.
